It’s my anniversary!
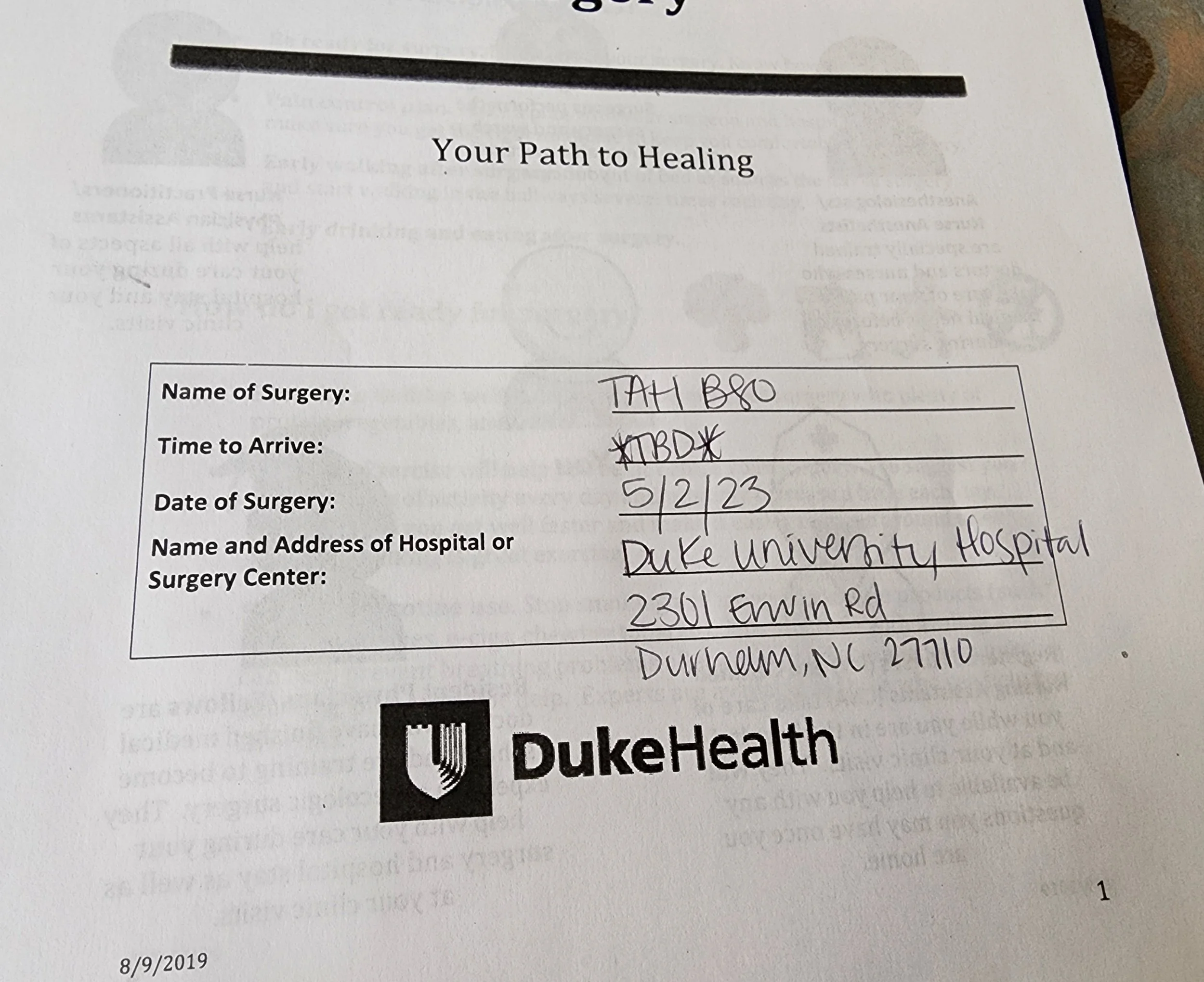
This journey began on May 2, 2019, when I had my first surgery here in Wilmington. Last year on this same date, I had my second surgery - the big surgery - at Duke University Hospital. Two life-changing surgeries. One date - 4 years apart.
How thankful I am for the excellent care I have received through the years and the kind support of family and friends through it all.
Today I am reflecting on the goodness of God, and I'll be listening to this "Just as Good" (Chris Renzema) on repeat.
And I will build an altar
And stack it stone by stone
'Cause every Ebenezer says I've never been alone
My faith will surely falter
But that don't change what You've done
'Cause every Ebenezer points to where my help comes from.
The April 22 appointments
I had three appointments at Duke on April 22. Here’s a quick update.
My first appointment was with Dr. Rossi at 10:30 a.m. We had a great visit as we talked about the present - and the future. I’ll have a CT scan at my next visit.
Then I went to the lab at 11:30 to test Inhibin A, Inhibin B, AMH, and to do a CBC.
These results were almost instant. We have no idea what was causing the low RBC Count before, but my RBC Count is fine now.
Then Rick and I had lunch at Pure Vegan, per the usual.
Cardiology was at 2:30 at the Raleigh location. It was a positive visit with Dr. Deepa Upadhyaya. She’s confident I do not have any major heart issues. She believes the accelerated heart rate I am experiencing when exercising might be a neurological result of the surgery last year, but just to be safe, she wants me to return for an exercise stress echocardiogram in July.
And today I received this amazing news. 🙌
I'm NED!!
Next up?
DXA Bone Density (to make sure Letrozole isn’t having an excessively negative effect on my bone density) and the ECHO Stress test -July 24
CT with contrast/ Dr. Rossi - August 12
Thank you to all of you have who been faithfully praying for me on this journey!
September 25 at Duke
As many of you are aware, I went to Duke September 25 for three appointments.
I’m going to start out by reiterating what I’ve said before. The standard of care at Duke is phenomenal. If I have to be a patient, I am thankful to be a patient at Duke.
8 a.m. Labs
Inhibin A
Inhibin B
AMH
I was seen on time, had a pleasant conversation with the woman drawing my blood, and was out the door in less than 10 minutes.
9 a.m. Dr. Rossi and Dr. Patel
This was a routine appointment since I don’t have any major complaints and labs were done for the first time post-op just an hour before.
We talked about the need for routine monitoring, and we agreed on doing a CT scan for January. It’s likely I’ll have CT scans every 3-6 months and blood work every 3 months for the foreseeable future.
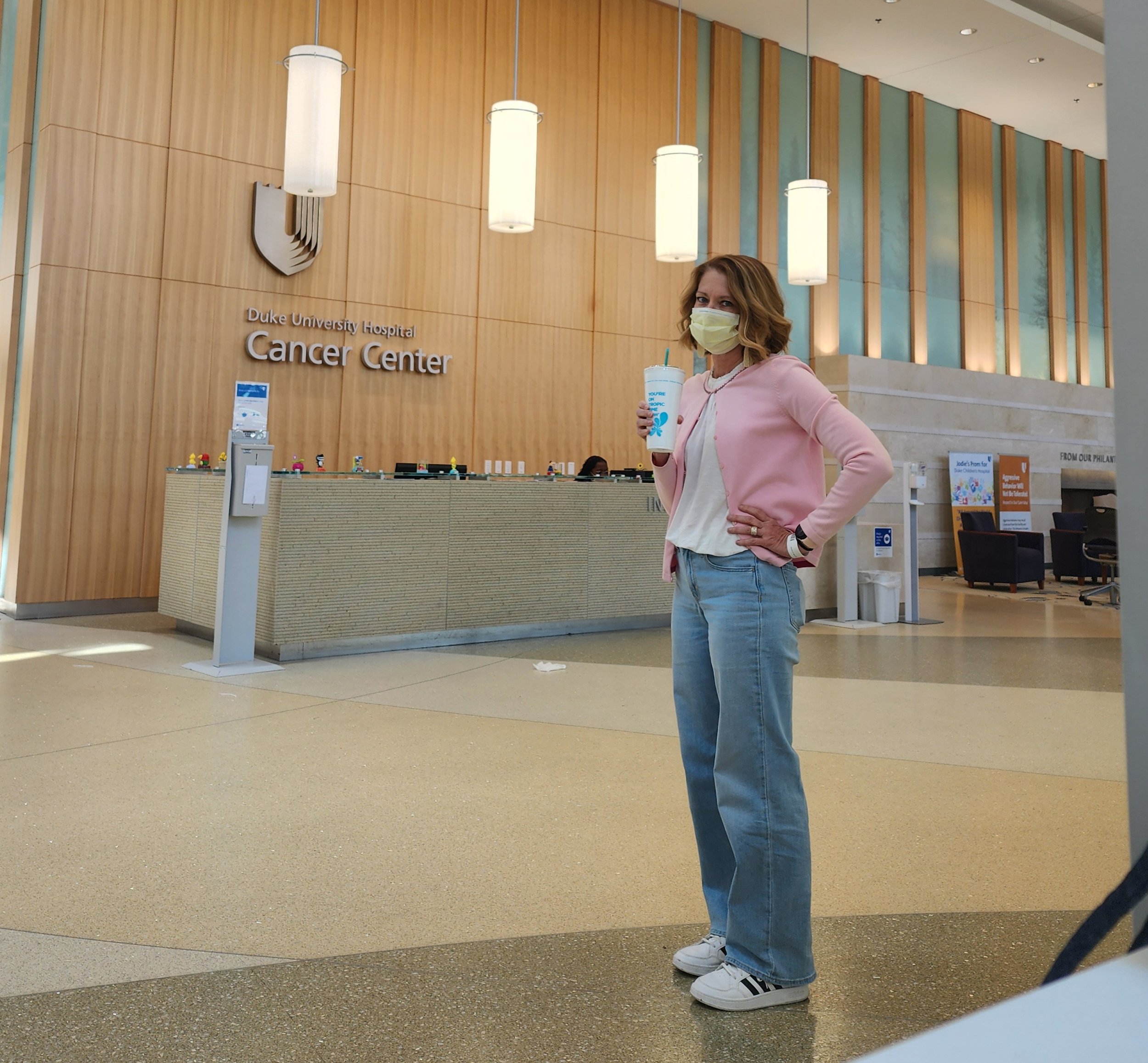
On my way to Duke for the first time back in April, I had my first Detox Island Green smoothie from Tropical Smoothie. I drank quite a few of those same smoothies while in the hospital after surgery, and because there’s a Tropical Smoothie in the Duke Cancer Center, I now feel like this smoothie is just a needful part of the whole routine.
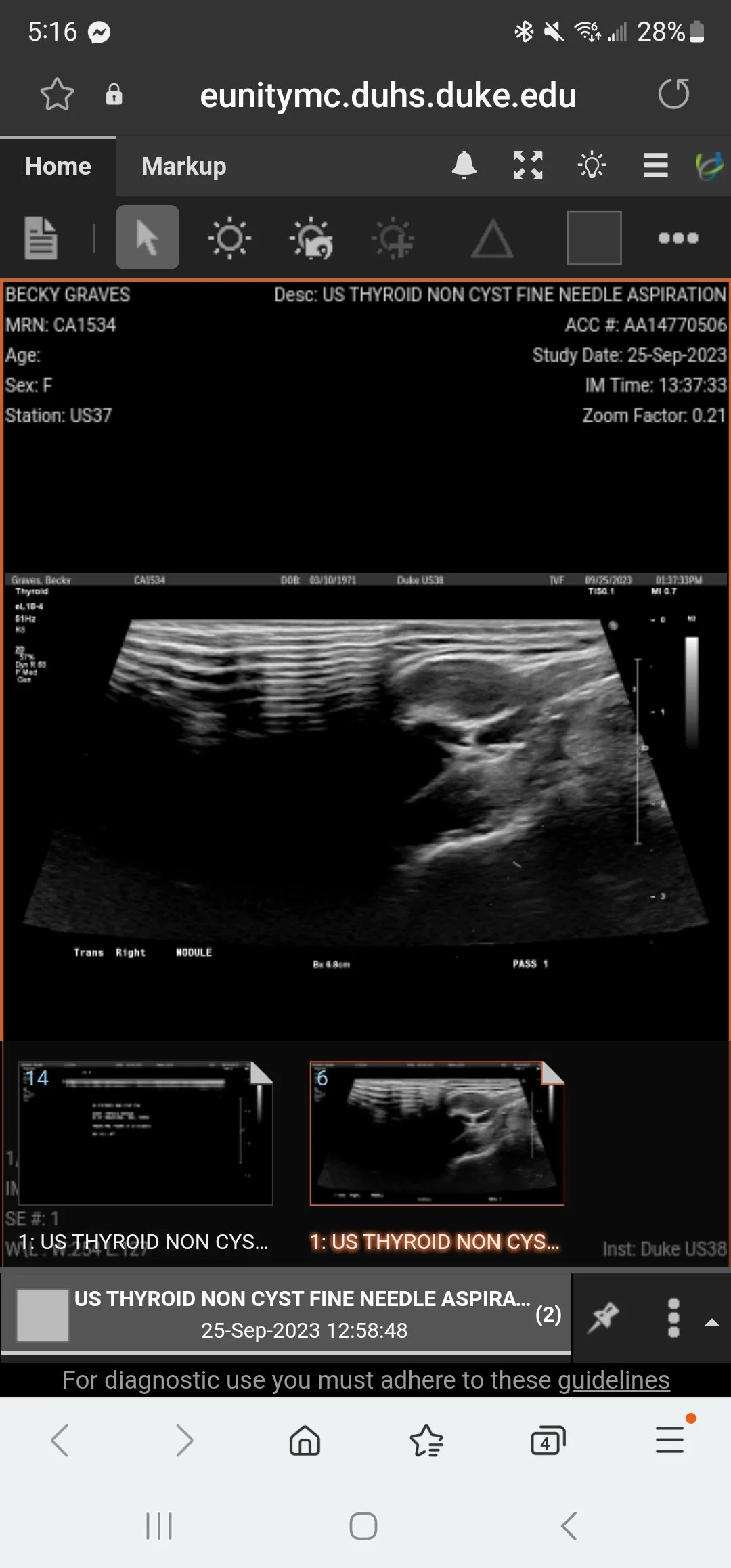
1 p.m. - Thyroid Biopsy
So, no one warned me. A thyroid biopsy is no joke.
I’m not kidding. The biopsy was more painful than anticipated, though in the grand scheme of things it doesn’t even compare with some of the things I’ve already done. Part of the issue was the Lidocaine did not work the way it was supposed to, plus they needed to go in three times - the 3rd time with larger needle. And I felt pain every single time they punctured the thyroid.
After they’d gone in the 2nd time and decided they need to go in a 3rd time, I had to ask for a short break to gather myself because I really thought I might pass out. Thankfully, I did not, and on the 3rd attempt they got an adequate sample.
Results
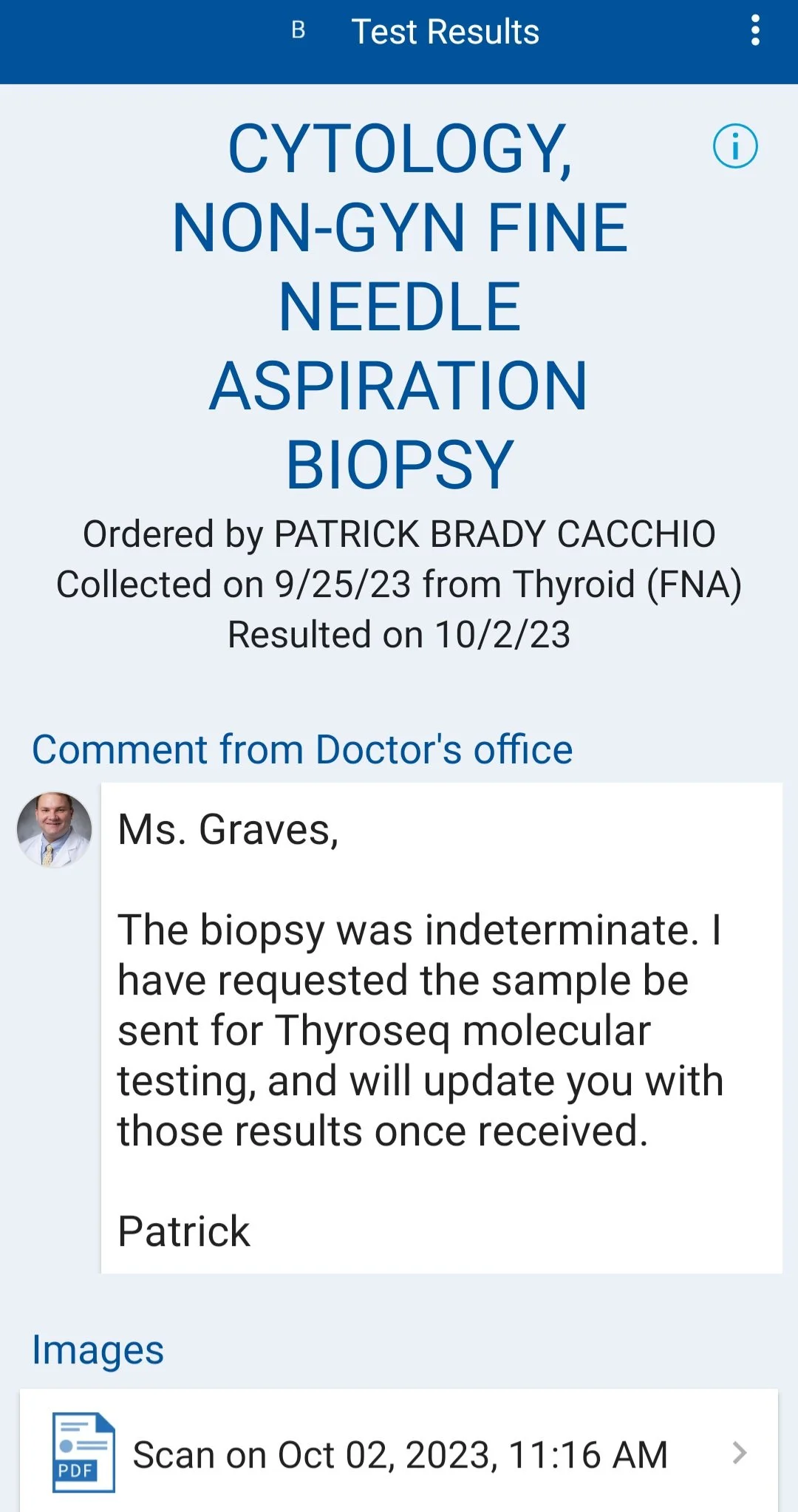
I waited to share this post until I had all results back.
Inhibin A - lowest number we’ve seen since I was first tested in 2019
Inhibin B - lowest number we've seen since I was first tested in 2019
AMH - - lowest number we've seen since I was first tested
Thyroid Biopsy - indeterminate. Being sent for further testing.
A slight change in plans
For those of you who have inquired and are praying, here’s an update.
I was able to get my thyroid biopsy moved to Duke on Monday, September 25, the same day I will have my first post-op labs and my 2nd post-op appointment.
Labs are at 8 a.m. I’ll see Dr. Rossi at 9 a.m. And then I will have the thyroid biopsy at 1 p.m.
That’s a quite a bit for a single day, but it definitely beats driving back and forth to Durham a second time, and it also assures all of my care will be at Duke and nothing can be lost between practitioners.
Thank you for caring and praying!
A different level of care
From scheduling to reception to nursing staff to physicians, the patient care I have received at Duke is far beyond anything I’ve experienced anywhere else.
I had my first appointment with endocrinology yesterday, and I was reminded again of all of the reasons I am thankful I transferred my care to Duke. I am exceedingly grateful for good insurance that allows me options and choices.
Our health care system as a whole is broken, but I can say without reservation that kindness, compassion, and professionalism characterize standard of care at Duke and make the long drives to and from appointments worth every mile.
My June 5th Post-op Appointment
Good morning, Everyone! I want to start out by saying thank you to everyone who reached out yesterday to check in, knowing I had my post-op appointment.
The appointment went as well as could have been expected. I really appreciate the team at Duke. Dr. Rossi has a wonderful ability to tell me the things I need to hear in a way that I can accept her recommendations. I know she has taken into account my thoughts on the matter.
We discussed at length the reality that 1) this was not my first surgery for GCT, 2) I had multiple malignant areas in my abdomen on May 2, 3) malignancy is likely to recur in the future, and 4) management is limited due to the unpredictable nature of granulosa cell tumor.
There is no perfect solution.
However, given where I am right now, we have decided that combining the drug Letrozole with routine testing and monitoring would be the best option.
No, I do not want to be on a prescription medication long-term, but taking all factors into consideration, Letrozole would seem to be the wisest course, even with all of the potential side effects that could come with it.
I have been researching Letrozole for the last month, discussing pros and cons with other medical professionals as well as women like myself with recurrent GCT.
If Letrozole works, it could hold the cancer at bay for a substantial length of time. If it does not, we can move on to other options.
Further, Dr. Rossi and I discussed my plan to continue being active and choosing the best food and supplement options.
In preparation for starting Letrozole, I will have a DEXA scan (bone density test) on June 16 in Raleigh, just to be certain I am at a good baseline for starting this medication as it could reduce the strength in my bones.
Again, there is no easy answer, but I am thankful I have choices. I am thankful for modern medicine. I am thankful for good health insurance that allows me to pursue multiple options. I am thankful for a community that has surrounded me and keeps showing up in so many ways to encourage me.
And I am thankful to know true Hope.
Above all that we could have asked or imagined
It wasn’t the worst case scenario. It wasn’t the best case scenario, either. It wasn’t even somewhere in the middle. It was even better than we asked or imagined.
It wasn’t the worst case scenario. It wasn’t the best case scenario, either. It wasn’t even somewhere in the middle. It was even better than we asked or imagined.
We arrived at the hospital a little before 5 a.m., and I was absolutely miserable. I had become dehydrated by the bowel prep, and this was causing extreme nausea and fatigue. So when I was called back to the pre-op prep area, I was relieved.
My new friend I met on the phone yesterday stopped by, as well as Dr. Rossi and other members of the surgical team. Every caregiver was so kind and compassionate.
The patient care here at Duke is phenomenal. One guy on the anesthesiology team was even showing me photos of his dog and chatting with me while another physician was doing my epidural in the OR.
I entered the OR at 7:27 a.m., and the surgery started at 8:50. The procedure was complete, and I was ready for visitors by 10:12 a.m. This was much shorter than the time originally estimated!
The shortened time under anesthesia resulted in a fairly quick stay in the recovery unit, and I felt aware of my surroundings and confident in my ability to communicate almost immediately. My first questions:
Do I have a bag?
Did she have to breach the abdominal wall to remove the tumors in the subcutaneous tissue?
The answers to both questions was “no!”
Further, Dr. Rossi decided not to do a hysterectomy, and there was no need to resection the bowel (that tumor was incredibly easy to remove!) so I came away from the procedure with a less invasive procedure than I had anticipated.
It looks like I’ll be here at Duke through Friday. I’ve yet to get out of bed. (That’s a goal for tomorrow!) I still have an epidural administering pain meds. (I’m not complaining!) And I have a great volunteer nurse. (Ethan is the best human!)
Tonight Ephesians 3:20-21 is on my mind:
“Now all glory to God, who is able, through his mighty power at work within us, to accomplish infinitely more than we might ask or think. Glory to him in the church and in Christ Jesus through all generations forever and ever! Amen.”
The last 24 hours
To those of you who have called, texted, and showed compassion in so many different ways, thank you.
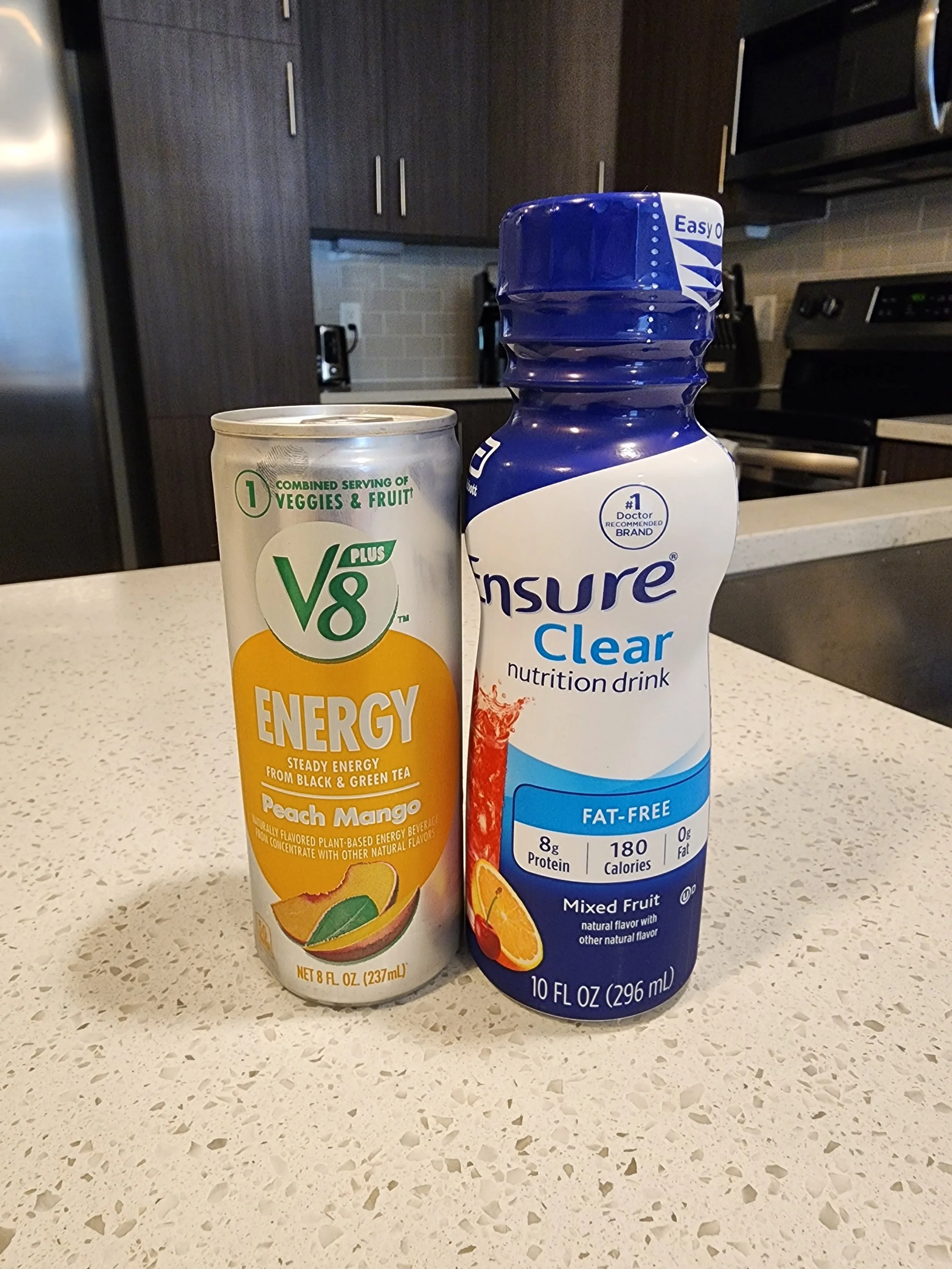
I’ve spent today walking and following the dreaded clear liquid diet - which hasn’t been nearly as bad as I anticipated.
Surgery is scheduled for tomorrow at 7:10 a.m.
Looking forward to sharing positive news as I feel able!
This is actually happening
My appointment at the Duke Cancer Center yesterday went as well as I could have possibly expected. I walked away with a firm plan, as well as confidence in the surgeon who will operate on me May 2.
I consented to a much larger surgery than originally anticipated, but the surgeon’s reasoning lines up with my goals for the future. I am at peace with the following:
Exploratory laparotomy
Total abdominal hysterectomy
Left-salpingo-oophorectomy
Debulking (removal of visible tumors)
Abdominal wall resection
Possible bowel resection
Possible ostomy
Actual surgery time will be set the day before the procedure. Expected hospitalization ranges from two days to one week.
At this point my medical team and I are in agreement that I will not have chemotherapy after the procedure, but if biopsies of different tumors reveal anything other than GCT, there is still the possibility that chemo could be warranted.
So, yes, there are still many questions about the future, but I do feel that I have finally found a firm plan with the expertise needed for my unusual situation.