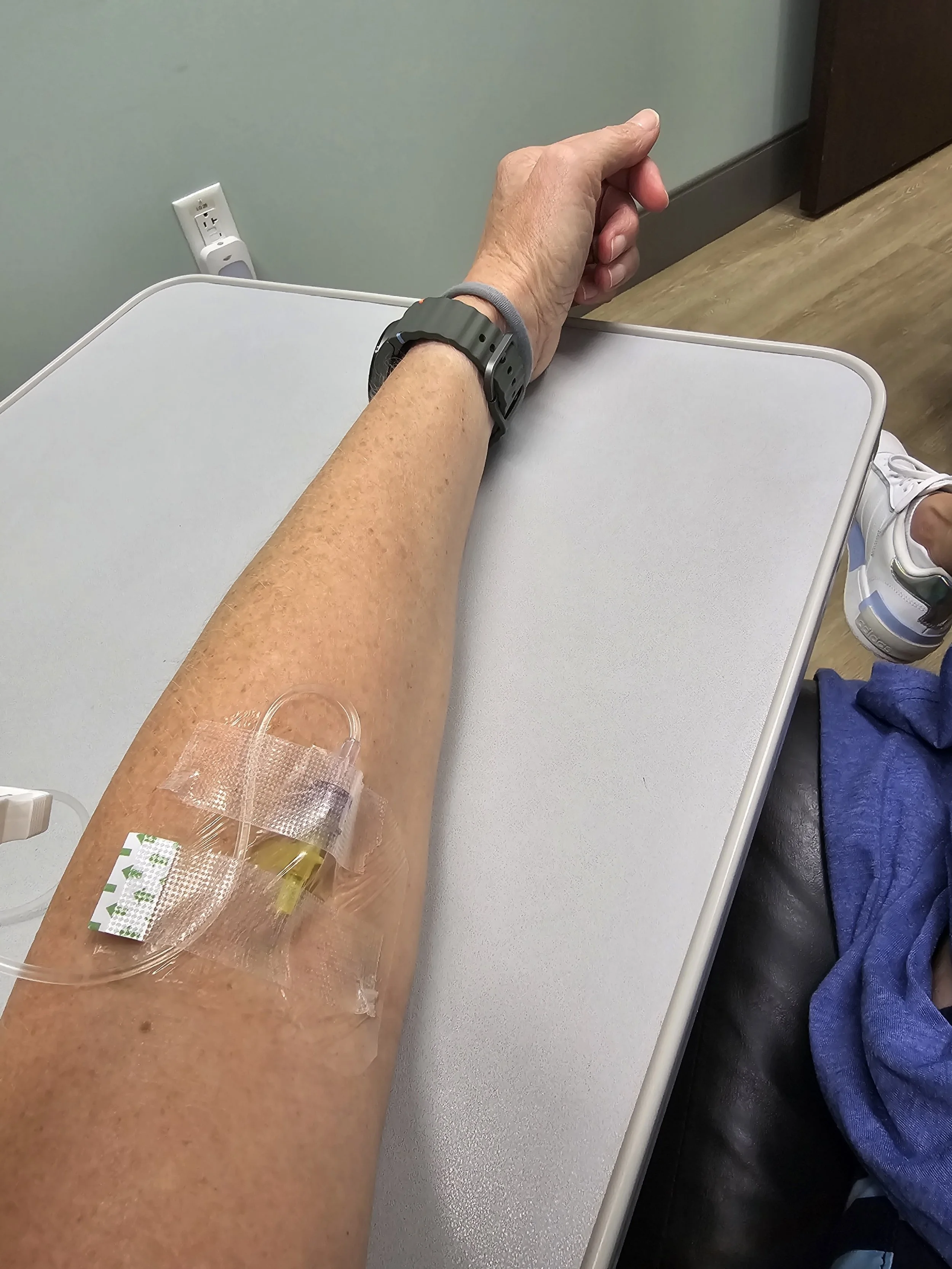
Reclast infusion
Yesterday I had a Reclast infusion. In July when the DEXA scan revealed significant bone density loss in just one year due to the use of Letrozole, I had a choice: stop taking Letrozole or do something to counter the negative impact Letrozole is having on my bone density. Since my August CT scan was clear (which we will assume is due in part of Letrozole), I chose to stay on Letrozole.
I then had another decision to make. Would I choose to take a weekly bisphosphonate, a monthly bisphosphonate, or a yearly infusion?
After careful thought and consideration, I chose the Reclast infusion because it seemed to fit in best with my lifestyle.
I was warned that this weekend I could potentially experience side effects, including:
Nausea
Vomiting
Arthralgia
Back pain
Bone pain
Dizziness
Fever
Fatigue
Flu-like symptoms
General weakness
Chills
5:30 am The only issue I am really dealing with is back pain, which although significant, is not keeping me from going on my beach walk soon
7:30 am Back from the beach and not feeling great. Back pain. Shoulder pain, Abdominal pain. Nausea. My calves feel like they do after a marathon.
9 am I feel I have the flu.
I spent the rest of the day in bed and never finished this post, but I woke up today (Sunday) feeling basically back to normal, so I hope the worst is behind me.
I’ll know in a year if this infusion and the discomfort that came with it was worth it.
The privilege of compassion
Suffering hadn’t shrunk their hearts, you see. It had expanded their capacity for compassion. The more stories of suffering I hear, the more I understand that our humanity places each of us on a spectrum of suffering...
Our experiences of suffering are best leveraged when they make us more aware of other people’s pain.
Suffering grants us the hard-won privilege of compassion.
Katherine Wolf, Treasures in the Dark
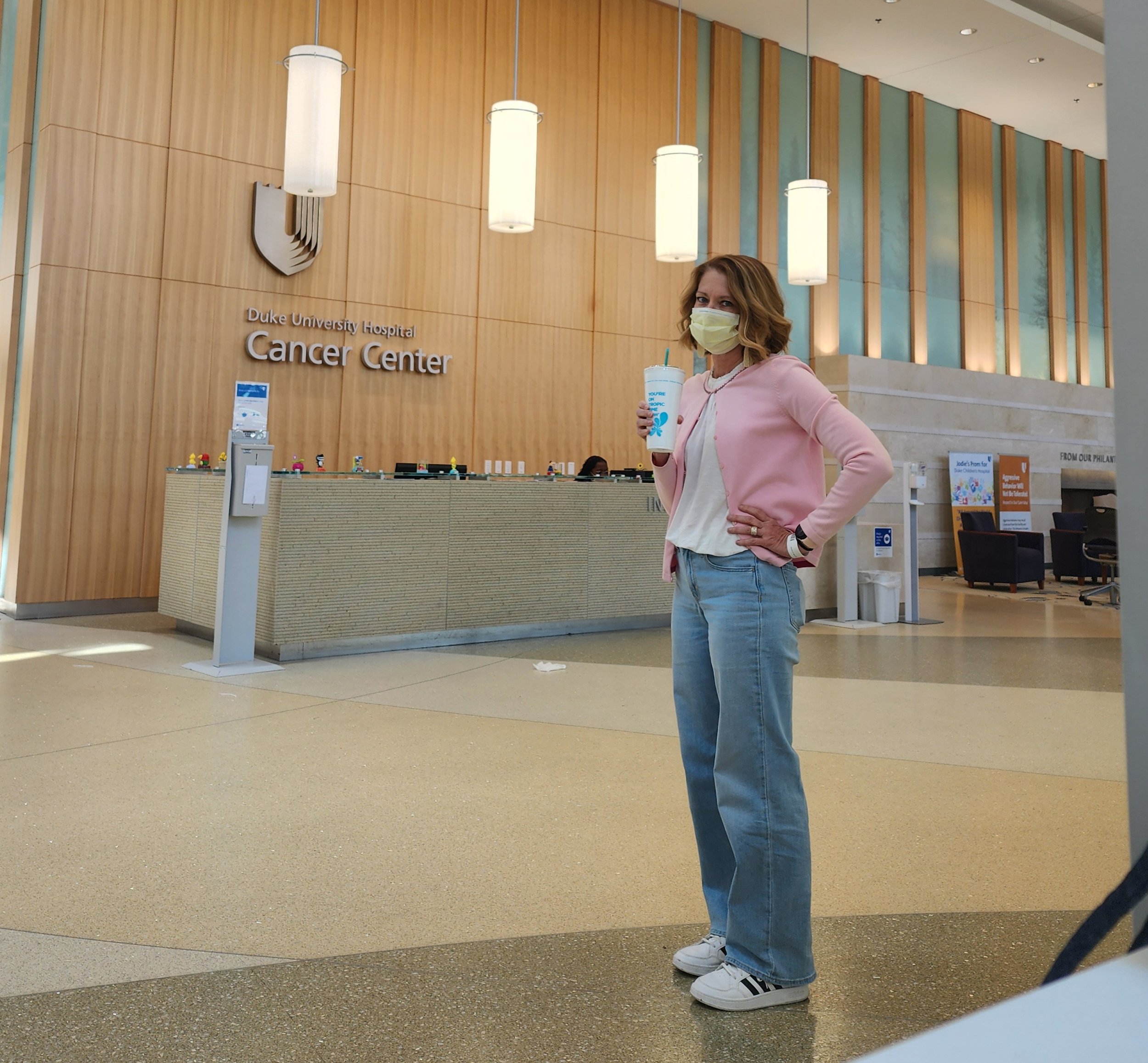
The April 22 appointments
I had three appointments at Duke on April 22. Here’s a quick update.
My first appointment was with Dr. Rossi at 10:30 a.m. We had a great visit as we talked about the present - and the future. I’ll have a CT scan at my next visit.
Then I went to the lab at 11:30 to test Inhibin A, Inhibin B, AMH, and to do a CBC.
These results were almost instant. We have no idea what was causing the low RBC Count before, but my RBC Count is fine now.
Then Rick and I had lunch at Pure Vegan, per the usual.
Cardiology was at 2:30 at the Raleigh location. It was a positive visit with Dr. Deepa Upadhyaya. She’s confident I do not have any major heart issues. She believes the accelerated heart rate I am experiencing when exercising might be a neurological result of the surgery last year, but just to be safe, she wants me to return for an exercise stress echocardiogram in July.
And today I received this amazing news. 🙌
I'm NED!!
Next up?
DXA Bone Density (to make sure Letrozole isn’t having an excessively negative effect on my bone density) and the ECHO Stress test -July 24
CT with contrast/ Dr. Rossi - August 12
Thank you to all of you have who been faithfully praying for me on this journey!
Nutrition and Lifestyle
You’ll find me at the beach every morning I’m here in Wimington.
A number of you have reached out recently to check in since I haven’t posted anything new since the January appointment. I haven’t posted anything because there’s nothing new to share. And that’s a really good thing!
Surgery went so well last year, so it’s likely I’ll be in this period of waiting between 3-month appointments for some time. GCT tends to be a marathon, not a sprint.
And, ironically, I’m running the Wilmington Half Marathon tomorrow because, truly, I feel great!
It has now been over a year since my recurrence was diagnosed, and consistently I hear from people things like, “You look great” or “You seem to be doing so well.”
And it’s true. I am doing so well.
The conversation then often turns to questions related to what I am eating and what lifestyle changes I’ve made in the last 12 months.
It is my opinion that the subject of nutrition and lifestyle is a complicated one, and I believe what is best for one person’s body is not necessarily what’s best for another person. However, this is where I am currently. I’m all about consistency, so it’s easy for me to share with you my typical routine.
I still have one cup of regular coffee every morning. The one change I have made is that I now put just the tiniest splash of half and half in it - no creamers, not even all-natural creamer.
I have a heaping tablespoon of almond butter (no added sugar or salt) every morning as my first food. Always. I even found some great individual packets that I can slip into my computer bag while traveling.
I do 30 minutes of weights, stretches, and yoga.
Then I go for a walk/run for 60 minutes or more depending on what my training schedule has for the day.
I come home and eat a banana, a couple of teaspoons of plain yogurt with a tablespoon of Seven Sundays Rise and Shine Mix. I also drink a ginger shot from Trader Joe’s most mornings.
The rest of the food I consume regularly can be characterized by these “rules”:
No pork, beef or poultry
Lots of fruits and vegetables
Minimal gluten, dairy, sugar or processed foods
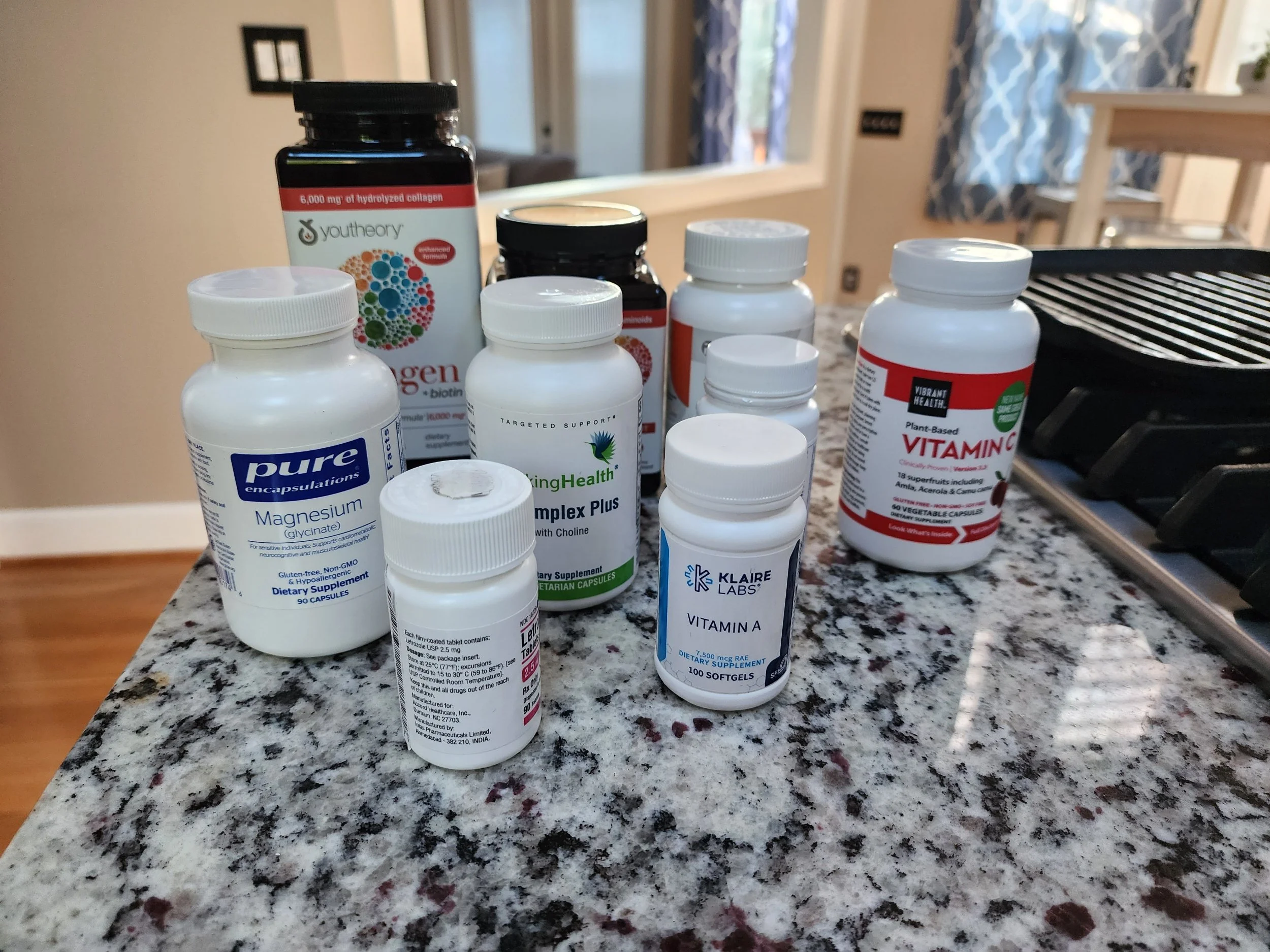
Though not food, supplements are a big part of my nutrition routine.
I have chosen to eat the way I eat and exercise the way I exercise because it’s a healthy lifestyle - whether or not one has cancer. I can tell you, though, it’s a lot easier to stick to the program knowing what I now know. A brownie isn’t really a temptation, and I don’t look for excuses for not exercising.
I go back to Duke April 22. Hopefully there really won’t be much to say after that appointment, either.
Until then I’ll continue to enjoy fresh produce that’s available year-round while eagerly anticipating fresh-picked strawberries and blueberries that are coming soon!
The wind & waves bring beauty
The last few mornings at the beach have been cold and windy, the waves pounding the shore, leaving very little room to walk on the sand.
I told a friend on Wednesday morning, “Just wait. This is going to bring some great treasures to find soon enough!”
Today I went to the beach filled with expectation, believing I would find something beautiful.
I walked north on Lumina from Johnny Mercer to Access 2. I then went out to the sand to head back, and almost immediately I spotted the first treasure of beauty. I didn’t really even have to search.
It was right there.
And that’s how the rest of the walk went. I saw beautiful treasures all around.
This caused me to think on my own journey over the last year, how at times the circumstances have been cold and unrelenting like the wind has been at the beach this week. And yet, for now, the winds have calmed and I see so much beauty every day. I am not even having to search for it.
It is right there.
Life is so beautiful.
Follow-up on supplements
I recently had labs done by my primary care physician. These were the regular, annual physical labs that include things like a Lipid Panel and a Comprehensive Metabolic Profile.
All of my results came back normal except for my Red Blood Cell count which is always low. Even my magnesium level, which was incredibly low in the past, is now normal. Other test results that were “off” before are now where they should be.
Is it the supplements? Is it the healthy eating? Is it both? We can not know for certain, but I do know that given the positive results, I’m going to continue on the road I am on.
We’re still waiting
Many of you have been kind to check in over the last few days to see if I have heard back from my thyroid biopsy. I have not.
Even though the biopsy was over three weeks ago, due to the initial inconclusive results, we’re now waiting on Thyroseq molecular testing results, and according to my provider in endocrinology, “The typical turnaround for the molecular testing is 2-3 weeks, so we hope to hear something this week or next.”
Thanks for caring, and thanks for praying. I appreciate your kindness. I’m becoming as anxious to hear as some of you are. Meanwhile, I’m here enjoying walks on these crisp fall mornings, balancing activity with the fatigue that comes when I overdo it, and listening to this song on repeat.
Happy Tuesday!
90 days with Letrozole
I share this information in hopes of helping someone else who is debating whether or not to go on Letrozole.
When I made the decision to begin taking Letrozole, both my physician and a number of women who are on the medication told me to expect:
Neuropathy in my hands and feet
Muscle or joint pain
Hot flashes
Night sweats
Edema
Dizziness
Weight gain
Loss of appetite
Digestive issues
Hair loss
Insomnia
Fatigue
Thus far, my experience with Letrozole, however, has been fairly easy, and given the potential for positive results, I am thankful that this is the treatment option Dr. Rossi and I agreed upon together. Of course, we won’t know about bone density loss for some time, but I am under the care of an endocrinologist who plans to monitor my bone density yearly, and for that I am thankful.
If I had to rank these side effects in order of how they have affected me, it would look like this:
Fatigue and insomnia. I have learned to take my medication no more than 30 minutes before I want to go to sleep because it definitely puts me to sleep. However, I often find myself waking up between 1 and 2 a.m., and it’s generally difficult to get back to sleep. This is probably why I often feel tired during the day, and I frequently take an early afternoon nap.
Neuropathy in my hands, feet and legs. I have experienced muscle and joint pain, as well, though not so much as to keep me from exercising. In fact, exercising has been my coping mechanism when it has been bad. Some days are worse than others, and mornings are generally worse than other times of the day. But it’s all bearable.
I’ve had my fair share of hot flashes and night sweats, but they’re more annoying than anything else. And, of course, I’d be having those anyway, even if I weren’t taking Letrozole.
Edema has been the latest annoying side effect. It’s becoming uncomfortable to wear my wedding band some days. But on other days, I don’t feel like I am swelling at all. I can not identify a pattern or causation. The edema I have experienced seems to be random.
I have not gained weight. In fact, I’ve been steadily losing weight. I think this is because of the diet I am choosing to eat (think rabbit food) and the fact that many days my appetite is less than it used to be.
Dizziness. I have low blood pressure, so I can’t say if this is any worse than it’s been before.
Digestive issues. I have not had many digestive issues, but I attribute that to my diet more than anything else. I have become a big fan of a cold pressed ginger juice with cayenne pepper, and exercise surely helps, as well.
Hair loss. I’m definitely experiencing this, though so far I think I am the only one who has noticed it. Again, this was to be expected after surgery, so I can not attribute it directly to Letrozole.
I share this information in hopes of helping someone else who is debating whether or not to go on Letrozole. As I have said before, each woman’s experience with GCT is different. This might not be the right option for someone else, but, for now, I believe Letrozole is the right option for me.
A slight change in plans
For those of you who have inquired and are praying, here’s an update.
I was able to get my thyroid biopsy moved to Duke on Monday, September 25, the same day I will have my first post-op labs and my 2nd post-op appointment.
Labs are at 8 a.m. I’ll see Dr. Rossi at 9 a.m. And then I will have the thyroid biopsy at 1 p.m.
That’s a quite a bit for a single day, but it definitely beats driving back and forth to Durham a second time, and it also assures all of my care will be at Duke and nothing can be lost between practitioners.
Thank you for caring and praying!
Good reminders and a beautiful sunrise
Walking the beach, listening to Craig Groeschel share the Word this morning.
A few gems:
The providence of God is best viewed backwards.
I want to remind you of the goodness of the God Who is able and Whose plan is always better.
So if you're stuck in the in-between, stay faithful to God.
While you are waiting, God is still working.
Groeschel referenced this passage of Scripture, a favorite of mine:
Now to Him who is able to do immeasurably more than all we ask or imagine, according to His power that is at work within us, to Him be the glory in the church and in Christ Jesus throughout all generations, forever and ever. Amen.Ephesians 3:20-21
You can listen to the whole sermon by clicking on the link below... or listen wherever you listen to podcasts.
It’s a delicate balance
Though each of us is living with GCT, we’re each on our own unique path.
When I was first diagnosed with Granulosa Cell Tumor in 2019, I did a fair amount of research on the subject, but I did not seek out community with others with the same condition.
However, when I was diagnosed with a recurrence in February of 2023, I immediately began searching out a support system, wanting to gather all the information I could before moving forward in making crucial decisions. I found a group of women on Facebook who have been a great support system, a wealth of information.
On the one hand, I am so thankful to hear the stories of others, to read about their experiences, to understand how they came to the decisions they have about their own care.
On the other hand, some days it gets to be a little heavy, hearing how difficult things are for some of my GCT sisters, wondering if my life will be like that in the days ahead.
It’s in those moments, when my mind goes to the “what ifs” I know I need to step back, to stop reading, to give myself room to breathe and remember every person’s story is unique. Though each of us is living with GCT, we’re each on our own unique path.
There's a delicate balance between being informed and being discouraged.
A different level of care
From scheduling to reception to nursing staff to physicians, the patient care I have received at Duke is far beyond anything I’ve experienced anywhere else.
I had my first appointment with endocrinology yesterday, and I was reminded again of all of the reasons I am thankful I transferred my care to Duke. I am exceedingly grateful for good insurance that allows me options and choices.
Our health care system as a whole is broken, but I can say without reservation that kindness, compassion, and professionalism characterize standard of care at Duke and make the long drives to and from appointments worth every mile.
Because I decided in March I was going to share this journey…
Here we go. I’ve gone back and forth about whether I was going to share this, but I’m going to put it out there . . . even if it turns out to be nothing . . . because it’s part of the journey.
Back in February when my recurrence was diagnosed, a thyroid nodule was noted on the CT scan. In all that transpired after that before finally having surgery in May, that little "concern" was put on the back burner.
Recently I realized, "Hey! That was never addressed. And hey! You've got to watch out for yourself because no one else is doing that for you."
So . . . a few weeks ago, I saw my PCP. He looked at the scan and suggested I see an ENT for an ultrasound of my thyroid. I finally had that appointment today.
Though I have a number of nodules (which is common), there is one large one which is solid with substantial intranodular blood flow that is "concerning." Therefore, I will have a needle biopsy on September 26.
The ENT was incredibly kind, and he wanted to make sure "this won't push you over the edge." He reminded me not to be worried until we have cause to be worried. So that’s what I am going with.
There’s nothing to worry about until there is something to worry about.
Functional Medicine
According to The Institute for Functional Medicine,
Functional medicine is a systems biology–based approach that focuses on identifying and addressing the root cause of disease. Each symptom or differential diagnosis may be one of many contributing to an individual’s illness.
For example:
One of the physicians who treated me this spring and affirmed my going on Letrozole also urged me to look into functional medicine to broaden my perspective on health and healing. Therefore, I have established care with a local practitioner.
Thus far, I have had one virtual appointment, one in-person appointment, blood draws that yielded 6 pages of results, and a recommendation to begin taking a number of supplements.
And honestly, at this point, I am not sure what my opinion is on it all.
My blood work was largely “unimpressive.” No one thing jumps out as being problematic. In fact, of the 84 results given, only 4 were outside of the reference interval -and only marginally so, at that.
The practitioner recommended adding some supplements to those I was already taking, so now my daily intake includes vitamins C, A, and a B complex, magnesium, melatonin, turmeric, and collagen with biotin, plus a-Drenal.
The bottom line is this. I do not expect my functional care practitioner to have the panacea, but at this point I feel like what she’s recommending can’t hurt, so I am willing to combine her recommendations with traditional treatment and a healthy lifestyle that includes physical activity and conscious eating.
The Fueled by Faith Podcast
My flesh and my heart may fail, but God is the strength of my heart. and my portion forever.
Psalm 73:26
I recently had the opportunity to talk to my friend, Emily, on her podcast - Fueled by Faith. Though the conversation was not what we had planned, we believe it is exactly what God intended for us both on a morning when we were both clinging to the promise of Psalm 73:26:
My flesh and my heart may fail, but God is the strength of my heart, and my portion forever.
A quick Thursday update
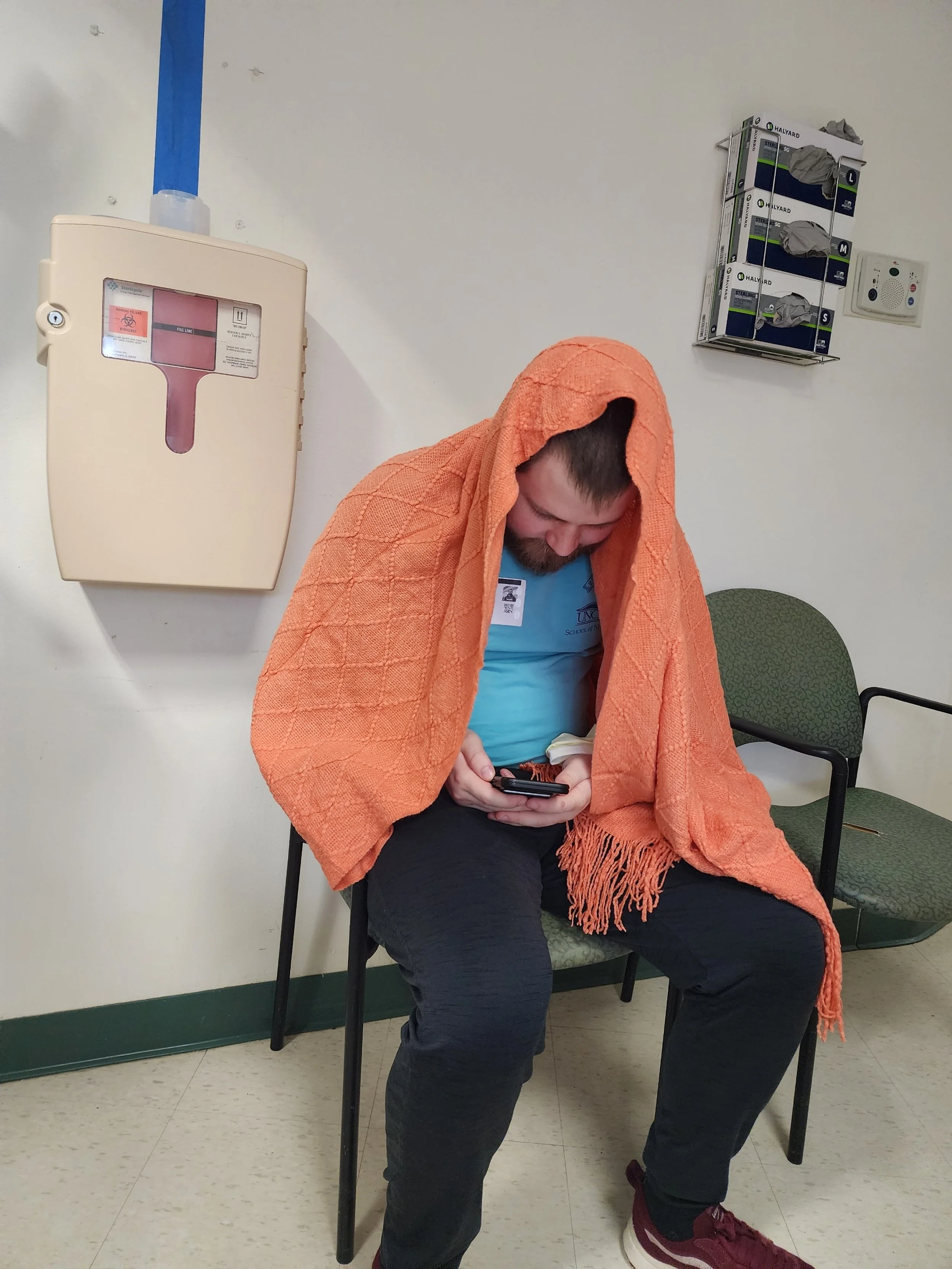
Wednesday went by quickly as I had several visitors and different teams were checking in on me every couple of hours.
I was able to get up and walk laps around my floor. There’s a board where we’re to keep track of our laps. I ended up at 3 miles at the end of the day. I’m room 6309. (Yes, I am bragging.)
Ethan has been a great help to me, even staying overnight. It’s been good having him here and seeing him put his professional skills into action on a personal level (and he really likes this blanket Elizabeth gave me).
Yesterday afternoon, however, we noticed I was experiencing some sort of allergic reaction (probably due to the epidural), so that was suspended, and I’ve only had Tylenol and Motrin since then.
My battle scars are substantial, but I am proud of them because they mean Dr. Rossi was able to do what she needed to do, and I came out on the other side.
I am hoping to be discharged later today (or at the latest, tomorrow), and I look forward to a clear plan going forward that includes healing and health.
I truly appreciate all of care and support that has come from so many of you. Thank you for being on my team during this unusual season.
Above all that we could have asked or imagined
It wasn’t the worst case scenario. It wasn’t the best case scenario, either. It wasn’t even somewhere in the middle. It was even better than we asked or imagined.
It wasn’t the worst case scenario. It wasn’t the best case scenario, either. It wasn’t even somewhere in the middle. It was even better than we asked or imagined.
We arrived at the hospital a little before 5 a.m., and I was absolutely miserable. I had become dehydrated by the bowel prep, and this was causing extreme nausea and fatigue. So when I was called back to the pre-op prep area, I was relieved.
My new friend I met on the phone yesterday stopped by, as well as Dr. Rossi and other members of the surgical team. Every caregiver was so kind and compassionate.
The patient care here at Duke is phenomenal. One guy on the anesthesiology team was even showing me photos of his dog and chatting with me while another physician was doing my epidural in the OR.
I entered the OR at 7:27 a.m., and the surgery started at 8:50. The procedure was complete, and I was ready for visitors by 10:12 a.m. This was much shorter than the time originally estimated!
The shortened time under anesthesia resulted in a fairly quick stay in the recovery unit, and I felt aware of my surroundings and confident in my ability to communicate almost immediately. My first questions:
Do I have a bag?
Did she have to breach the abdominal wall to remove the tumors in the subcutaneous tissue?
The answers to both questions was “no!”
Further, Dr. Rossi decided not to do a hysterectomy, and there was no need to resection the bowel (that tumor was incredibly easy to remove!) so I came away from the procedure with a less invasive procedure than I had anticipated.
It looks like I’ll be here at Duke through Friday. I’ve yet to get out of bed. (That’s a goal for tomorrow!) I still have an epidural administering pain meds. (I’m not complaining!) And I have a great volunteer nurse. (Ethan is the best human!)
Tonight Ephesians 3:20-21 is on my mind:
“Now all glory to God, who is able, through his mighty power at work within us, to accomplish infinitely more than we might ask or think. Glory to him in the church and in Christ Jesus through all generations forever and ever! Amen.”
Sunrise on a Sunday morning
I love my early morning walks here in our neighborhood. This is the last one for a while as we leave for Durham later today in order to prepare for my surgery at Duke on Tuesday.
This morning was quite ordinary - listening to Russell Moore’s podcast, then worship music.
The future is so uncertain, but I will heed this solid advice I've received:
Don't look left. Don't look right. Look straight ahead, and follow Jesus.
Amen.
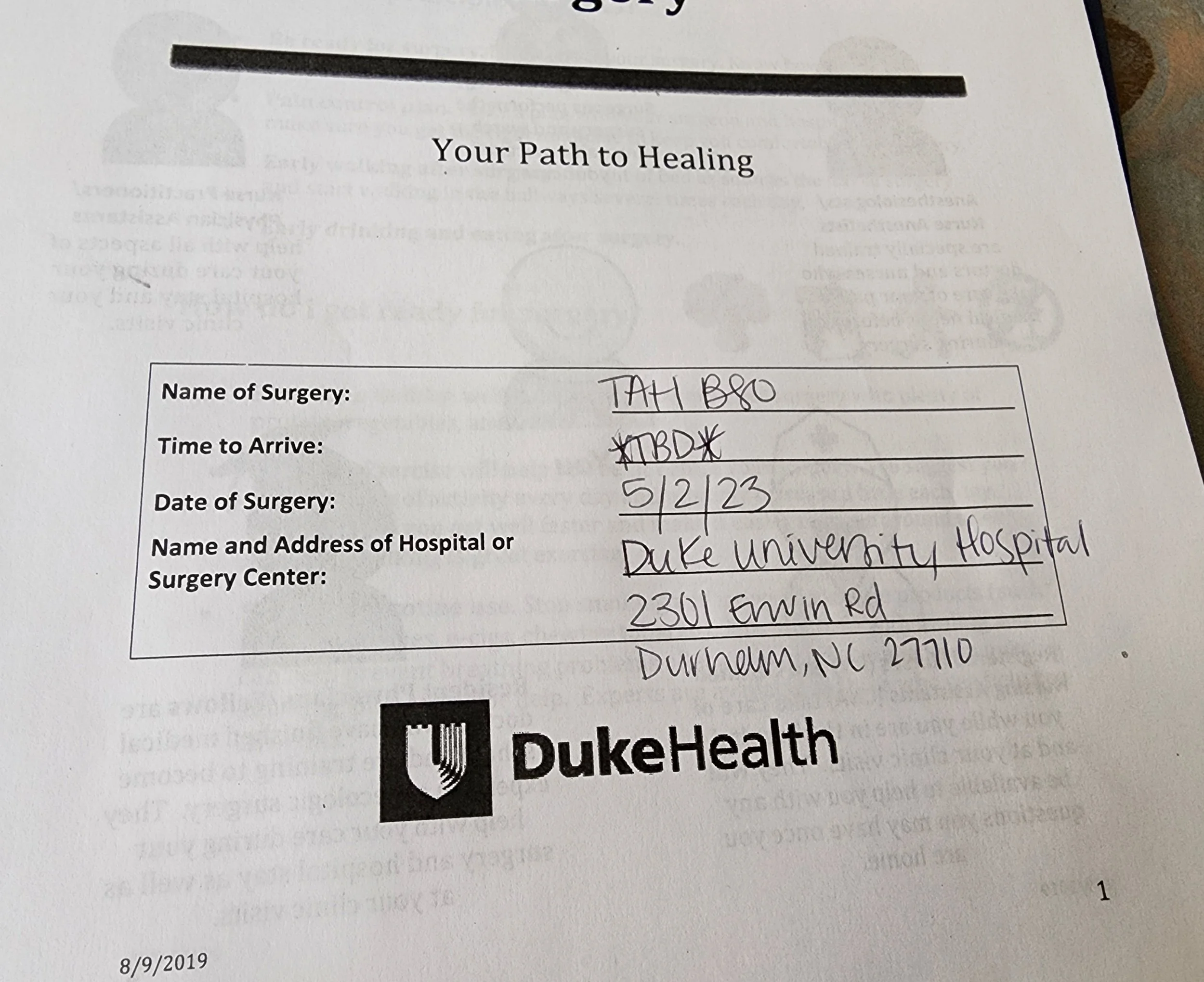
This is actually happening
My appointment at the Duke Cancer Center yesterday went as well as I could have possibly expected. I walked away with a firm plan, as well as confidence in the surgeon who will operate on me May 2.
I consented to a much larger surgery than originally anticipated, but the surgeon’s reasoning lines up with my goals for the future. I am at peace with the following:
Exploratory laparotomy
Total abdominal hysterectomy
Left-salpingo-oophorectomy
Debulking (removal of visible tumors)
Abdominal wall resection
Possible bowel resection
Possible ostomy
Actual surgery time will be set the day before the procedure. Expected hospitalization ranges from two days to one week.
At this point my medical team and I are in agreement that I will not have chemotherapy after the procedure, but if biopsies of different tumors reveal anything other than GCT, there is still the possibility that chemo could be warranted.
So, yes, there are still many questions about the future, but I do feel that I have finally found a firm plan with the expertise needed for my unusual situation.
A quick update
I had more bloodwork today - a new test. It’s a good thing I have good veins. I’m giving blood frequently these days.
The conversation with Dr. J in Australia was encouraging and productive. Because of that phone call, it is the current “new plan” to forego chemotherapy because there's no real evidence it actually has any measurable benefit in preventing recurrence of GCT.
I’ll have a mammogram, ultrasound, and biopsy tomorrow.
I have canceled surgery for April 14 here in Wilmington because…
I have an appointment at Duke on Monday, and I hope to schedule surgery at Duke in the near future.
All of this just moves me one step closer to resolution and a firm new plan.